The Introduction of Abdominal Pain
Definition
Abdominal pain refers to pain below the stomach and above the pubic symphysis.
Corresponding diseases in CWM
Abdominal pain is a common clinical symptom occurring in many digestive diseases, like enterospasm, pancreatitis, gastrointestinal neurosis, enteritis, and colitis. It caused by gynecological conditions will not be covered in this chapter.
Etiology
EPF invasion
- Cold congeals and leads to stagnation.
- Summer Heat combines easily with Damp to block Qi circulation.
Emotional frustration
- Anger and worry may cause Liver-Qi stagnation → LR overacts on SP → Blood stasis → abdominal pain.
Improper diet
- Too much spicy, heavy, flavored food → Damp-Heat.
- Too much cold, raw food → damages Spleen-Yang.
- Eating too much → food retention → abdominal pain.
- Chronic food retention in children → abdominal pain.
- Unclean food → food poisoning.
- Worms → generally Damp-Heat in character.
Trauma/surgery
- Causes Blood stasis, which blocks abdominal meridians.
Yang deficiency constitution
- Fails to warm the Qi and Blood, creates internal Cold, which congeals Qi and Blood flow, leading to abdominal pain.
Pathology
- Many Zang-Fu organs are located in the abdomen. Many meridians run through the abdomen: ST, SP, LR, GB, KI, CV, Dai Mai, and Chong Mai. Any Zang-Fu organ damage or meridian blockage may lead to abdominal pain. Blockage of Qi movement and the meridians is the chief pathology for excess patterns, while malnourishment of the Zang-Fu and meridians creates deficiency patterns. Overall, the most commonly seen causes of abdominal pain in the clinic are Cold invasion, Qi stagnation, and food retention.
- The organs involved in abdominal pain include SP and ST, LR and GB, KI and BL, SI, LI, TE.
- There is inter-transformation between excess and deficiency. For example, long-term Cold pain can turn into Heat; Qi stagnation can turn into blood stasis; deficiency pain is easily invaded by pathogenic factors; trauma/surgery leads to Blood stasis, which in turn leads to Qi stagnation if Blood blocks Qi passage.
How to Diagnose and differentiate Abdominal Pain (see Table 7)
Differentiation of disease
(1)Stomachache
- Location of pain is higher — just below the Heart (abdominal pain is from below the stomach to above the pelvis.
- Accompanying symptoms include belching, acid regurgitation, nausea, and vomiting (abdominal pain uncommonly presents with belching and in this case many Zang–Fu could be involved).
- The main organ involved is ST and may relate to LR and SP.
(2)Dysentery
- Often combines with abdominal pain.
- Accompanying symptoms: rectal tenesmus, and diarrhea mixed with red and white mucus.
- Is an infectious disease.
(3)Gynecological disorders
Abdominal pain caused by gynecological conditions is usually located in the lower abdomen. It is closely associated with Menstruation, Leukorrhea, and Pregnancy.
Key points for differentiation
(1)Acute
- Severe pain.
- Accompanying symptoms caused by EPF, food retention, or parasites.
(2)Chronic
- Dull pain.
- Accompanying symptoms caused by internal injury or by Yang deficiency.
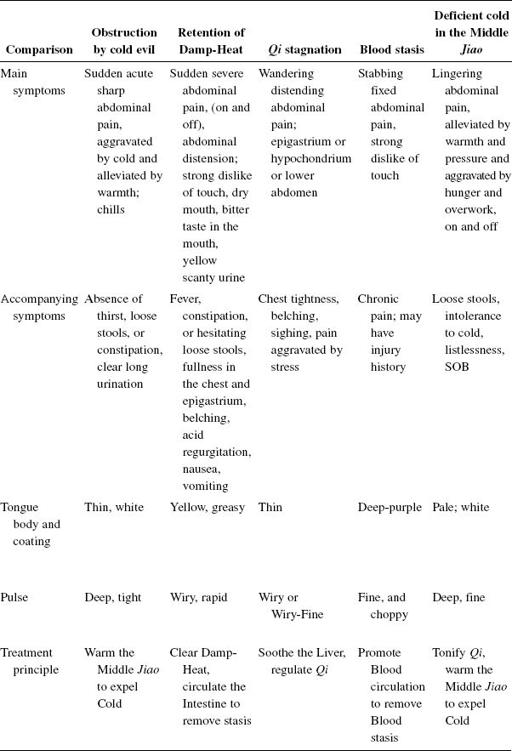 Table 7.Differentiation and treatment of abdominal pain
Table 7.Differentiation and treatment of abdominal pain
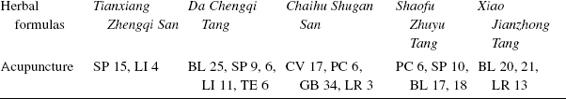
Basic points: CV 12, ST 25, CV 6, ST 36/37, SP 4.
(3)Deficiency
- Likes pressure.
- Not fixed.
- Dull pain.
- Pain with hunger.
(4)Excess
- Dislikes pressure.
- Fixed.
- Severe pain.
- After meals.
(5)Heat
- Severe acute pain and abdominal distension.
- Constipation.
- Fever.
- Thirst.
- Pain alleviated by cold.
(6)Cold
- Acute pain, not intermittent.
- Aggravated by cold.
- Alleviated by warmth.
(7)Qi Stagnation
- Intermittent, distending abdominal pain.
- Wandering pain.
(8) Blood Stasis
- Stabbing pain like that caused by a knife, or colicky pain that is fixed in location.
- Blood stasis signs on the tongue and pulse.
(9)To determine the organ involved:
- Pain in the whole area (except epigastric) — SP, ST, LI, SI.
- Pain in the sides of the lower abdomen — LR.
- Pain directly below the umbilicus — KI, BL.
- Pain around the navel and vomiting of clear water — parasites (worms).
Treatment
Principle of treatment
(1)Unblock the meridian
- Remove the pathogenic factor(s) for excess, e.g. clear Heat, transform Damp, regulate Qi, move Blood, or promote digestion.
- Tonify Zheng Qi for deficiency, e.g. warm the Middle Jiao, or tonify Qi and Blood.
Acupuncture
(1)Main points
- CV 6, 12
- ST 25, 36, 37
- SP 4
(2)Obstruction by cold
- SP 15
- LI 4
- CV, SP, ST, LI Meridians
- Reducing method and moxa
(3)Damp-Heat
- LI 4, 11
- SP 6, 9
- BL 25
- TE 6
(4)Qi stagnation
- CV 17
- PC 6
- GB 34
- LR 3
- PC, LR, GB, ST, and CV Meridians
- Even method
(5)Blood stasis
- PC 6
- SP 6, 10
- BL 17, 18
(6)Deficiency cold
- LR 13
- BL 20, 21
- CV, Back Shu, Front Mu
- Tonify and moxa
Severe hypochondriac pain → LR 14.
Upper abdominal pain → CV 12.
Pain around the navel → CV 6, 10.
Acid regurgitation (GB 34).
Thirst (ST 44).
Cold limbs (moxa CV 8 to warm the body).
Auricular acupuncture
- Large Intestine
- Small Intestine
- Stomach
- Spleen
- Shenmen
- Sympathetic
2 or 3 points.
Needles (10–20 min) or seeds.
Cupping
- Around abdominal points and Back Shu points
- 3 or 4 points each time
- 1 or 2 times each day
Especially good for Cold or food accumulation.
Herbal
For Cold pain:
Xiaohuixiang (9 g) + Wuyao (6 g)
For Qi stagnation:
Wuzhuyu (3 g) + Muxiang (2.5 g)
For Qi deficiency:
Huangqi (15 g) + Gancao (licorice) (5 g)
Suggestions
- Avoid cold, raw food, especially in summer.
- Avoid camping in cold, wet areas.
- Avoid strenuous exercise after meals.
- Eat regular meals.
- Clean and cook vegetables.
- Do not eat too much greasy food.
- Increase meal frequency to decrease meal size.
- Regulate emotions.

