The Introduction of Stomachache
Definition
Pain in the epigastric region is called stomachache or epigastric pain. It is called Wei (Stomach) Tong (pain) in TCM.
Clinical features
Stomachache is often accompanied by other digestive symptoms, like nausea, vomiting, acid regurgitation/heartburn, belching, or poor appetite.
Corresponding diseases in CWM
- Chronic or acute gastritis.
- Peptic ulcers (gastric and duodenal ulcers).
- Gastric neurosis.
The Etiology of Stomachache
- Invasion of Cold in the Stomach which causes stagnation of Stomach-Qi, and further leads to Blood stasis or turns into Stomach-Heat.
- Overeating, especially overeating cold and raw food, sweet and greasy food, spicy food, or overdrinking alcohol impairs the Spleen and Stomach in transportation and transformation, producing Damp retention.
- Emotional frustration involving anger, anxiety, and depression damages the Liver, causing Liver-Qi stagnation and Liver-Fire flaring-up, which overacts on the Stomach and pain arises.
- Aging or long-term illness lowers the functions of the Spleen and Stomach, causing deficiency Cold in the Middle Jiao. Warm Diseases damage Yin, leading to Stomach-Yin deficiency.
The Pathology of Stomachache
Stagnation of Stomach-Qi is the chief Pathology for stomachache. It is caused not only by Stomach disorder, but also Liver and Spleen Pathology . The acute stage usually belongs to excess patterns, while the chronic stage turns into deficiency or mixed excess with deficiency patterns.
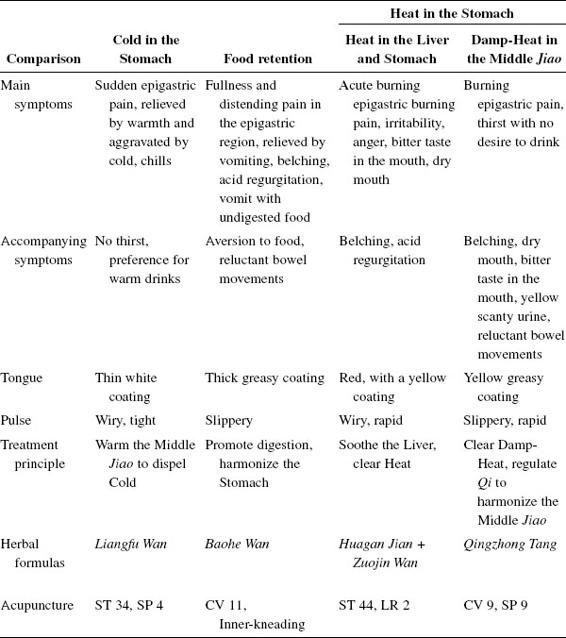
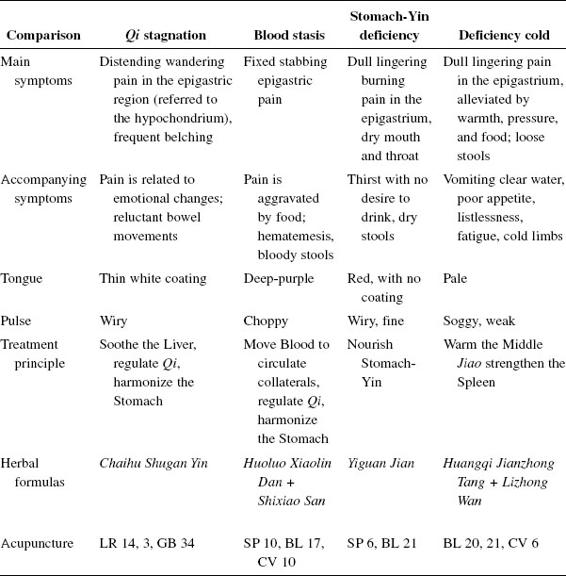
How to Diagnose and differentiate Stomachache(see Table 14)
Disease differentiation
(1)Cardiac pain
- Region affected.
- Severity (cardiac pain is more severe, with a more sudden onset, and may radiate to the left shoulder and neck as well as the PC 8 and HT 8 area; it may also be accompanied by sweating).
- Medical history.
- Accompanying symptoms.
Basic points: CV 12, PC 6, ST 36, 21.
(2)Stomachache
- Region affected by initial pain.
- Accompanying symptoms.
(3)Abdominal pain
- The area affected is larger (around or below the navel).
Basic points: CV 12, PC 6, ST 36, 21.
Differentiation of syndromes
(1)Determine excess or deficiency
Excess: distending pain, constipation, strong dislike of touch or pressure, pain being worse after a meal, overflowing pulse, severe fixed pain, new disease affecting a young person, tonification (improper treatment) making it worse.
Deficiency: no distension, no constipation, pain with preference for touch, pain being worse before a meal, weak pulse, wandering pain, chronic pain or dull pain, chronic disease affecting a weak person, reduction (improper treatment) making it worse.
(2)Determine cold or heat
Cold: acute, severe pain that is aggravated by cold and alleviated by warmth.
Heat: burning pain that is aggravated by heat and alleviated by cold; a yellow greasy tongue coating; a wiry, rapid or soggy, rapid pulse.
(3)Determine if it is affecting the Qi level or the Blood level
Qi stagnation: distending pain, belching, wandering pain; early stage.
Blood stagnation: stabbing pain, fixed pain; chronic stage.
The Treatment of Stomachache
Principle of treatment
Regulate Qi to harmonize the Stomach.
For modifications depending on the specific pattern, see the chart.
Acupuncture
(1)Main points
CV 12, PC 6, ST 36, 21
(2)Modifications
- ST 34 (Xi-cleft point) if there is severe pain.
- GB 34 if there is Stomachache.
- ST 44 (Jing-Spring point) to clear Heat if there is a bitter taste in the mouth.
- K I3 if there is burning pain in the Stomach (due to Yin deficiency).
- SP 10 if there is blood in the stools.
- BL 17 if there is vomiting of blood.
Moxibustion
Use in cases of deficiency Cold.
(1)Good points
- CV 12, 6, 4
- ST 25, 36
- P 6
Moxa stick: use for 5–10 min daily; 10 treatments = 1 course.
Moxa with ginger or aconite: moxa 5–7 units.
Auricular acupuncture
- Stomach
- Spleen
- Shenmen
- Subcortex
- Sympathetic
- Endocrine
Three or four points each time.
Scalp acupuncture
Use gastric lines, and retain the needle for 30 min. Electro-acupuncture is applicable.

